WHO’s Transformative initiative enhances healthcare for refugees in Rohingya Camps
4 March 2024
In the heart-wrenching reality of Rohingya refugee camps in Bangladesh, accessing healthcare became a labyrinthine ordeal marked by scarcity and uncertainty. Individuals faced a myriad of health challenges, ranging from infections to chronic diseases, with no discernible route to urgent medical attention. This complex struggle for adequate healthcare emerged as a central issue for improvement, catalyzing a transformative initiative championed by the WHO-led Health Sector.
This initiative emerged as a beacon of hope, bringing together an array of stakeholders including WHO, UNHCR, IOM, other health partners, local authorities, and law enforcement. With a clear goal in mind – simplifying the intricate referral system – the aim was to guarantee timely, life-saving care for the refugees. Amidst these concerted efforts, patients and healthcare providers emerged as the primary beneficiaries of this collaborative venture.
Previously, the Rohingya refugees faced overwhelming challenges in navigating the healthcare system that was new to them. Without clear referral criteria, inadequate communication, transportation hurdles, and incomplete feedback mechanisms; delays, frustrations, and sometimes poor health outcomes were not uncommon.
Hasina, a 35-year-old mother of four, suffers from high blood pressure and Diabetes Mellitus (high sugar level) and later developed a stroke that necessitated urgent hospitalization. She was worried about hours of waiting, multiple approvals, and the arduous task of arranging expensive transportation amidst security checkpoints and traffic snarls. "I was sure I was going to die," she recalls, overwhelmed by desperation and uncertainty. Hasina's subsequent referral experience portrayed the initiative's efficacy. Expedited approval, facilitated transportation, and dedicated accompaniment to the hospital that provided her with timely specialized care, igniting feelings of hope and gratitude. “I felt like I was given a new life. I felt optimistic and joyful.”
Using its convening powers, the WHO-led Health Sector rallied the strategic commitment and support of UNHCR and IOM in a collaborative approach with other health sector partners, the government of Bangladesh to a mutually agreed Patient Referral Standard Operating Procedures (SOP). This SOP outlined an efficient and effective way of working and the functionality of the referral system to target the recurrent operational problems and priorities of all constituencies. It tackled the issues of definition of responsibilities, expectations, and accountability, standardization of services at each level of care, collaborative monitoring, field-based decision support, and control systems through the medical referral committees.
Dr Shahin, a 45-year-old physician- working at IRC- was deeply involved in designing the initiative and praised its effectiveness in streamlining workflows and improving inter-professional relationships. “The initiative improved our relationship and cooperation with other healthcare providers and stakeholders,” says Dr Shahin. “It also increased our confidence and competence in providing quality care to our patients,” he adds.
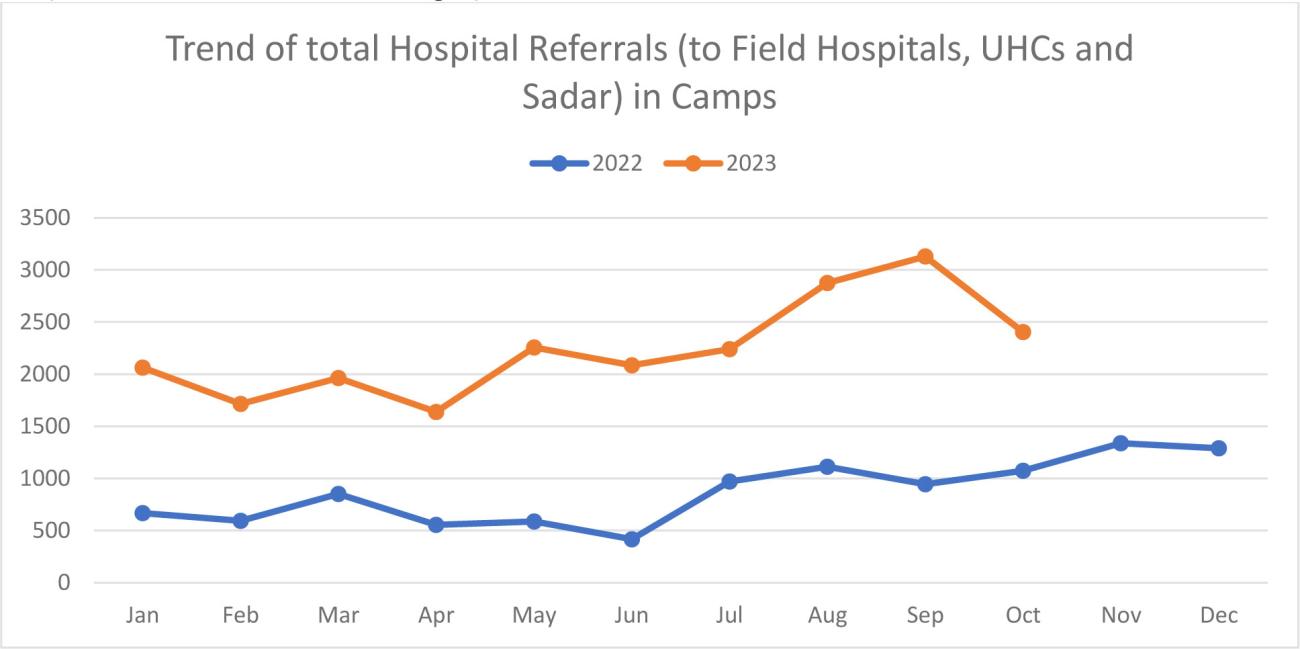
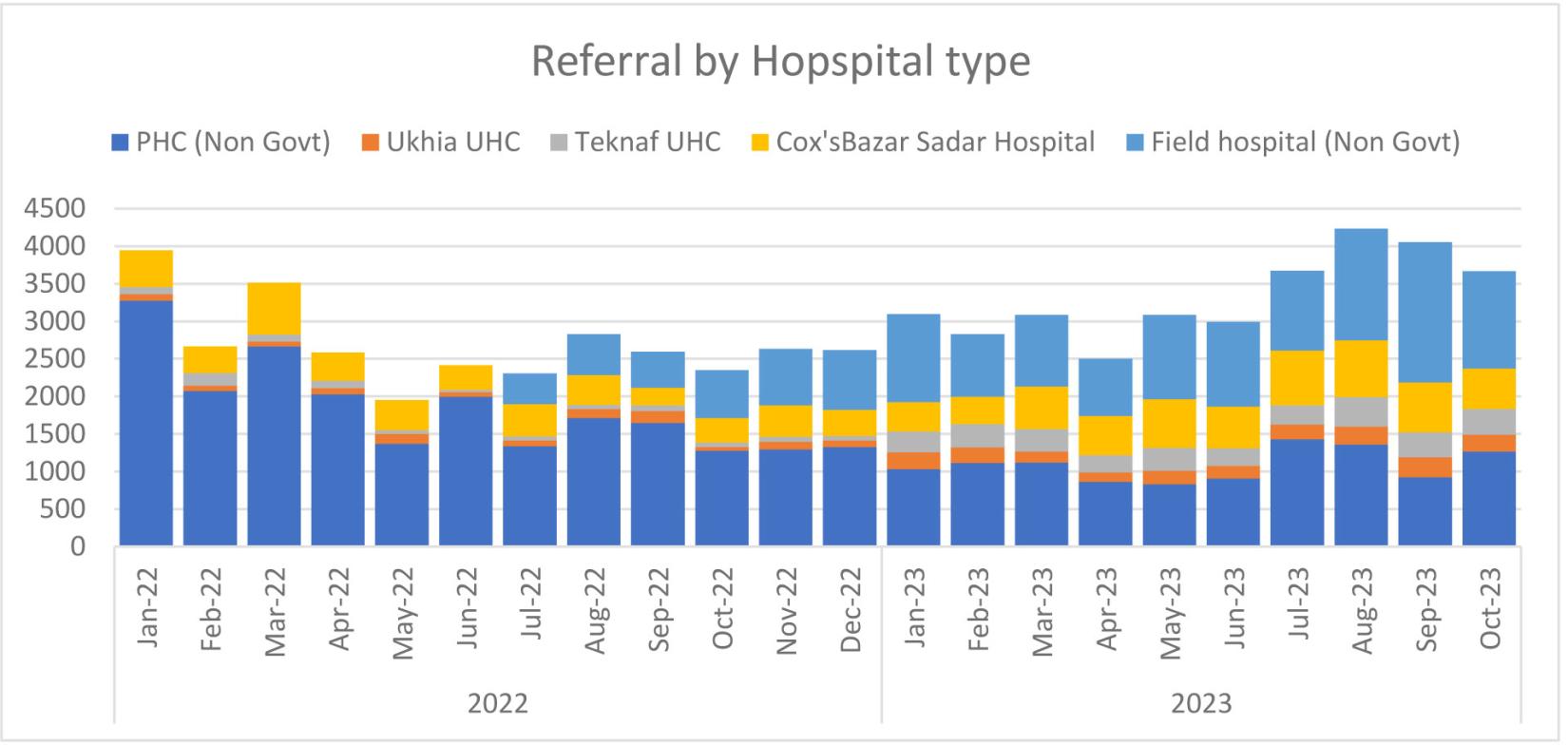
The initiative has streamlined the patient referral process and ensured timely care for those in dire need. This transformation also bolstered transparency, accountability, and a sense of shared responsibility among healthcare providers and patients alike. Statistical data post-implementation showed remarkable improvements: a 115% (10,400 in 2022 to 22,374 in 2023) increase in trends of total hospital referrals as shown in the graph below.
Dr Francis Tabu, Health Sector Coordinator at WHO Bangladesh, hailed the initiative's success in simplifying the referral process, ultimately saving lives, and nurturing trust among stakeholders. “The current referral system developed under the leadership of the WHO-Health Sector, operationalized largely with the support of UNHCR and IOM continues to be one of the most reliable mechanisms in facilitating straightforward access to secondary healthcare for the Rohingya refugees,” says Dr Tabu.
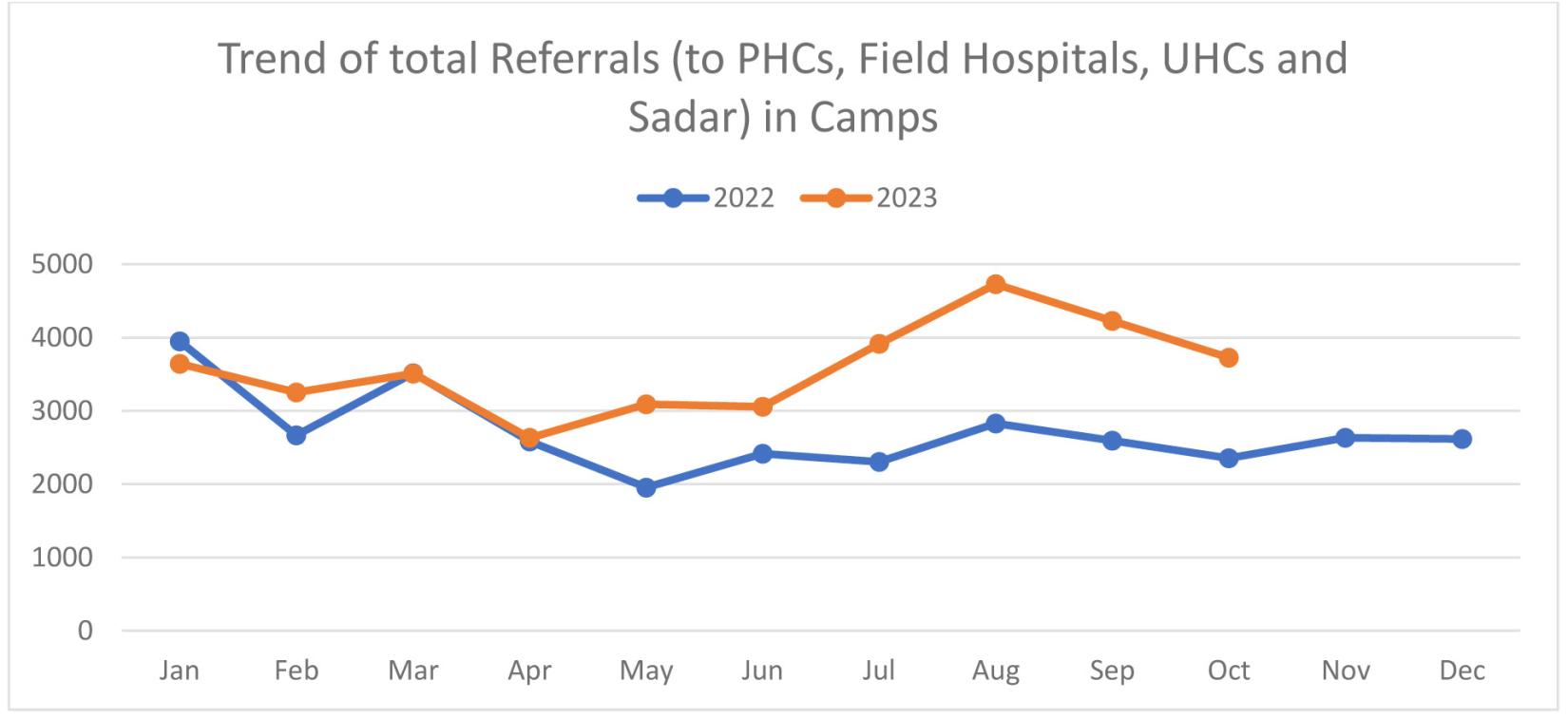
Source: Health Sector 4W Report Jan 2022 to Oct 2023
However, challenges persist due to limited resources and the unpredictable nature of humanitarian crises. Dr Jorge Martinez, Head of the WHO Sub Office in Cox’s Bazar, praised the role of communication, coordination, and transparency in improving healthcare, saving lives, and enhancing health outcomes. He also recognized the ongoing obstacles that the initiative faced, such as security threats that disrupted the referral process, population movements that changed the needs and demands of the patients, and environmental hazards that damaged infrastructure and resources. “The project also encountered some challenges that hindered its implementation and sustainability,” says Dr Martinez.
Looking ahead, the Health Sector Initiative remains steadfast in fortifying healthcare for Rohingya refugees. Its focus remains on continual evaluation, resource mobilization, and sustained collaboration to ensure enduring high-quality healthcare services.
For more information about the publication please contact Terence Ngwabe Che chet@who.int Ext. Communications Officer, Cox’s Bazar Office, WHO Bangladesh.



